The story of mitochondrial replacement therapy shows how ethically tricky genetic manipulation is becoming.
When scientists discover a new way to prevent disease or overcome infertility, they usually get applauded. But throw genetic engineering into the mix and it gets dicey fast. Genetic engineering in reproductive medicine is particularly scary because we’re talking about changing the genes of future generations — so any new technique is sure to incite controversy, especially in the United States.
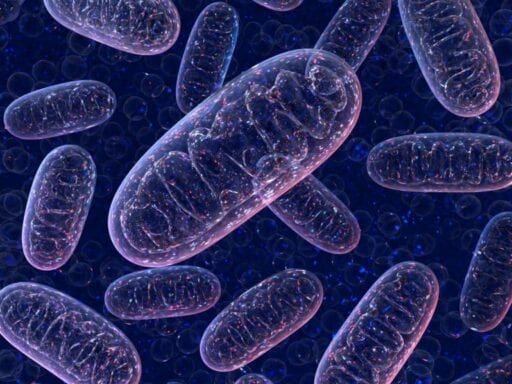
That’s what’s happened with a relatively new procedure that doctors have begun using to help couples avoid passing down genetic mutations that cause mitochondrial disease to their children. (For those of you who haven’t read about the mitochondria since high school, a refresher awaits you below.)
This mitochondrial replacement therapy, or MRT, has made headlines for producing “three-parent babies” because it involves replacing the mitochondrial DNA of an embryo that has a risk of mitochondrial disease with healthy mitochondrial DNA from a donor, or the “third parent.”
The mitochondria are essential to almost every cell in our bodies, so diseases caused by mutations in mitochondrial DNA can be extremely debilitating, with symptoms including seizures, developmental delays, blindness, and organ failure.
“The goal [of MRT] is very simple: It’s to prevent the birth of children who would be wheelchair-bound and oxygen-starved and are doomed to a slow, painful death, and whose parents must be going through hell,” said Eli Adashi, a professor at Brown University who specializes in reproductive biology. “It’s not that complicated.”
But when it comes to defining and regulating MRT, there’s considerable disagreement. Is it just another form of in vitro fertilization, or is it an early form of gene editing that could quickly lead to riskier attempts at human enhancement?
In 2015, the United Kingdom became the first (and so far only) country to officially legalize the procedure, strictly to prevent genetic disease. And this February, doctors at the Newcastle Fertility Centre in the UK performed the therapy on two mothers. Australia and Singapore, inspired by the UK, are now in the process of legalizing it.
In the US, research on the experimental procedure has been banned since 2015 due to a rider that was furtively added to an appropriations bill. The ban has been baffling to scientists, most of whom consider the procedure worth studying.
Yet it hasn’t stopped one US doctor, John Zhang, who runs a fertility clinic in New York City, from performing MRT in Mexico for a couple. And a clinic in Ukraine is partnering with Zhang’s clinic to offer this procedure to Americans who can afford the $15,000 fee.
MRT has garnered its fair share of criticism, given that it involves manipulating an embryo, which changes the genes of future generations of humans. And so far, only a handful of babies have been born using MRT over the past two years, which means we don’t yet know if there will be any long-term effects on them.
But since MRT is not so far removed from other fertility treatments, some scientists believe that it simply needs more research and proper regulation to become commonplace, perhaps even an IVF option for lesbian couples who want to have children genetically related to both of them.
With gene therapy and gene editing technologies like CRISPR giving us increasing power to change the DNA of future generations of humans, the story of MRT shows us the kinds of conversations we need to have surrounding these ethically tricky therapies.
So how does it work? Should we be scared of it? And why did it get banned in the US? Here’s what we know.
Mitochondrial DNA, explained
You may recall that the mitochondria are called the “powerhouse” of the cell. That’s because they float around in all our cells with the main function of producing high-energy molecules (called ATP) that fuel most processes in our bodies. But mitochondria are especially interesting because they have their own DNA.
About 99.9 percent of our DNA is housed in the cell nucleus as chromosomes. That extra 0.1 percent is located — you guessed it — in our mitochondria.
/cdn.vox-cdn.com/uploads/chorus_asset/file/11731505/536px_Mitochondrial_DNA_lg.jpg) National Human Genome Research Institute/Wikimedia Commons
National Human Genome Research Institute/Wikimedia CommonsWhen eggs are fertilized by sperm, you get a nucleus with DNA that’s half from the mom and half from the dad. But the sperm’s mitochondria don’t enter the egg, so the new baby cell only gets the mom’s mitochondrial DNA. In other words, our mitochondrial DNA is only passed from mother to child, a pattern known as “maternal inheritance.”
/cdn.vox-cdn.com/uploads/chorus_asset/file/11731515/43611_evo_resources_resource_image_362_original.gif) University of California Museum of Paleontology’s Understanding Evolution
University of California Museum of Paleontology’s Understanding EvolutionThe inheritance of mitochondrial DNA is not as well-studied as the inheritance of nuclear DNA, but we do know that if a mother has certain mutations in her mitochondrial DNA, it increases the risk of a child having severe disease.
From three people to one embryo
So how does mitochondrial replacement therapy work? To be clear, it is not exactly gene editing because doctors are replacing DNA that lies outside the nucleus. Instead, it falls under the umbrella of genetic manipulation.
While the nucleus of one of our cells contains about 30,000 genes, our mitochondria contain just 37 genes. These genes only code for proteins involved in making ATP, the molecule that provides energy for most of our cellular processes.
Just like our other DNA, our mitochondrial DNA can mutate, leading to the production of faulty proteins. Those faulty proteins can cause neurological diseases like Leigh syndrome, which is caused by damaged brain tissue, and MERRF, which results from abnormal muscle and nerve cells.
An estimated one in 5,000 people have mitochondrial diseases stemming from DNA mutations. Using data from 2012, the researchers at Newcastle University estimated that 12,423 women in the US are at risk of passing down mitochondrial diseases.
Mitochondrial replacement therapy offers a solution for mothers who may not want to pass down their mitochondrial DNA. Instead, a female donor’s mitochondria are used. So even though the popular phrase used to describe the treatment is “three-parent baby,” the resulting embryo only has a tiny bit of DNA from the donor. A child born from MRT has 99.9 percent of its DNA from its two parents.
There are a few ways of transferring mitochondria, but the two most common methods of doing MRT are pronuclear transfer and spindle transfer. It gets a bit complicated here.
In pronuclear transfer, both the maternal eggs and the donor eggs are fertilized via IVF. The fertilized nucleus (known as the pronucleus) of the donor egg is destroyed and replaced with the fertilized nucleus of the maternal egg, which has the DNA of the mother and the father.
In spindle transfer, the nuclear DNA from the mother (known as a spindle) is transplanted into the donor’s egg, replacing the donor’s DNA. This new egg is fertilized by the father’s sperm via intracytoplasmic sperm injection, a technique that’s similar to IVF, except the sperm is directly injected into an egg rather than entering the cell on its own in a petri dish.
Pronuclear transfer is the easier and cheaper method since the pronucleus is larger and easier to image and transfer than the spindle. But it also poses some moral and religious questions because it involves the destruction of fertilized nuclei, which some may consider akin to abortion (all the donors’ nuclei are fertilized and replaced).
Scientists at the Newcastle Fertility Centre use pronuclear transfer, while Zhang’s clinic uses spindle transfer.
The UK hospital has been pretty quiet about the procedure — the press office told Vox that it could not grant interviews yet — but the Guardian has reported that it’s done the procedure on two women.
Why MRT is banned in the US
Today, it’s illegal to perform MRT in the US, while the UK is at the forefront. But most of the research behind MRT — and the first baby born using the technique — was a result of the work of American scientists and doctors.
In 2009, researchers at the Oregon National Primate Research Center successfully performed MRT in a Rhesus macaque monkey. Follow-up studies like this one and this one concluded that MRT had the potential to be performed in humans.
With all this data backing up MRT, it was considered for approval from the Food and Drug Administration at the beginning of 2015. The FDA requested that a committee from the National Academy of Sciences review the procedure, and the committee published a report essentially saying that with oversight, MRT could be justified.
Progress on this front came to a halt when Congress passed the Consolidated Appropriations Act of 2016. Among other things, the bill included a rider that banned germline modifications. This term encompasses all genetic engineering on eggs, sperm, or early embryos — modifications that would be passed down beyond a single generation.
This law is why editing the genes of embryos is illegal, and it was likely included in the act because of increasing concerns over the ability of technology like CRISPR to one day allow us to engineer “designer babies.”
But there’s a big difference here: MRT gives us significantly less control than CRISPR over an embryo’s genes because the mitochondria only hold about 0.1 percent of our DNA. Yet since MRT involves changing the DNA in an egg, the rider also made MRT illegal. It’s unclear which Congress members included this rider, but it has been renewed every time and remains in the 2018 iteration of the act.
Jeffrey Kahn, director of the Johns Hopkins Berman Institute of Bioethics, was the chair of the committee at the National Academy that reviewed MRT before the 2016 act was passed. He was in charge of the report that justified MRT. “The week that we delivered our report to the FDA … the budget bill got passed,” he said. “The general counsel said the recommendations that we made would violate the prohibition.”
For now, women in the US don’t have any domestic options to prevent passing down their mitochondrial mutations to their kids. To get around the restrictions, Dr. Zhang took a couple to Guadalajara, Mexico, in 2016 to perform MRT for them. And then he got a letter from the FDA notifying him that he was breaking the law.
So while MRT has now become popular in the UK, its application in the US is still up in the air.
“[MRT] can technically be construed as germline modification, so mitochondrial replacement got swept up into that rider,” said Brown University’s Adashi. “It was caught up in the gene editing concerns, and I think it’s sort of an unfortunate linkage.”
“It was really an American idea,” he continued. “Which makes it all the more unfortunate that it has been restricted here.”
The big ethical question
Germline modifications — or changes to DNA in eggs, sperm, or early embryos — are controversial because they can theoretically involve altering future generations of humans. Especially in situations where regulations are minimal — or nonexistent, such as in Ukraine — giving scientists the ability to change the germline can be dangerous.
CRISPR, a powerful method of gene editing, was used to modify an embryo in 2017. In response, scientists published a statement in Cell, essentially saying that while research on genetic modification shouldn’t be prohibited, it should have proper oversight. These debates are important because we should be aware of the power of our science.
“Obviously, there are ethical considerations,” Adashi said. “Everybody’s always concerned about state-led eugenics, knowing what happened in World War II.”
Eugenics is the idea that humans can be selectively bred to create a perfect species. It reached an infamous nadir with the Nazi movement to create an “Aryan race” by wiping out people with undesired traits. It has a pretty dark history in the US as well.
But going from MRT to eugenics is a bit of a leap, particularly because the mitochondria only have 37 genes, which mostly lead to proteins specifically involved with metabolism.
“One has to be open to all possibilities, but it just seems rather far-fetched,” Adashi said. “That’s not to say you shouldn’t think about it; I just find it really a stretch to think something like eugenics will come from this.”
Most scientists agree that genetic modification makes sense to prevents certain heritable diseases from being passed down. As Kahn puts it, they don’t believe the germline is “inherently inviolable.”
“If the safety and uncertainty and precision concerns can be addressed, then germline modifications can be admissible and even preferable,” he continued. “Especially for diseases like Huntington’s, which is very, very heritable.”
In 2014, Marcy Darnovsky, executive director of the Center for Genetics and Society, wrote an op-ed in the New York Times explaining why MRT shouldn’t become legal. She noted that more than the scientific considerations, it’s the ethical issues that are more worrisome. Why should a woman undergo this experimental therapy, when safer alternatives such as in vitro fertilization or adoption exist?
“Simply being able to do something doesn’t mean we should do it,” she wrote.
But while the US banned it, lawmakers in the UK had a different approach to addressing the ethical concerns behind MRT. The Human Fertilisation and Embryology Authority (HFEA) — a branch of the UK’s Department of Health that specifically regulates fertility treatment and research — assembled a committee to review the scientific evidence backing up MRT. They incorporated public opinion and held debates in Parliament. In 2015, the HFEA permitted “cautious use of mitochondrial donation in treatment.”
Each patient in the UK who undergoes MRT must get a license from the HFEA. And there are strict guidelines for which women are allowed to have MRT: There must both be a risk of “mitochondrial abnormalities caused by mitochondrial DNA” in the egg and “a significant risk that a person with those abnormalities will have or develop a serious mitochondrial disease.”
/cdn.vox-cdn.com/uploads/chorus_asset/file/11731649/shutterstock_245325091.jpg) Shutterstock
ShutterstockAdashi considers the UK’s method for licensing MRT the gold standard of how to adjudicate difficult ethical questions.
“Britain has always been more pragmatic, more secular, less preoccupied with some of the things that we tend to place a great deal of value into,” he said. “We’re the last Western nation preoccupied with the ‘pro-life/pro-choice’ issue.”
Darnovsky and the FDA consider MRT to be similar to embryo editing via CRISPR — a change to the human germline, and therefore worthy of concern. But scientists in favor of MRT and the HFEA believe it to be more like in vitro fertilization, a fertility treatment that does not change the nuclear DNA. Turns out this difference in definition is the key to whether it’s accepted.
The future of MRT in the US
Adashi calls mitochondrial DNA “sort of a Wild West” in the study of heredity because there’s a lot about it that we still don’t know.
For example, we’re not certain why the DNA in our mitochondria typically mutates at a much lower rate than our other DNA. We also don’t really know how mitochondrial disease gets passed from mother to child; at this point, it seems random.
More importantly, as it pertains to the outcomes of MRT, what could happen to a child who has donor mitochondrial DNA that comes from a different source than nuclear DNA? Since mitochondrial replacement has only happened over the past few years, we don’t know the long-term effects yet.
But in order for this research to be done, the rider needs to be changed, since it currently prohibits anyone from even applying to the FDA to research MRT in humans.
“People are not going to be doing a ton of research if there’s not a pathway to humans,” Kahn said. “But there is interest in going forward; all it requires is someone taking [the ban] out.”
Earlier this year, Adashi co-authored a paper in Obstetrics and Gynecology explaining his belief that the ban on MRT research should be removed.
Rampant and unregulated MRT is not on the table. In fact, it’s quite the opposite. Scientists want regulations to be eased so that more research can be done on these unanswered questions about MRT; so that it can be carried out safely for those who really need it.
“Humanity has always needed time to get over scientific breakthroughs,” said Adashi. “The fear about revising the laws of nature, altering the natural order — it’s resistant to cerebral arguments. It generally takes a generation or so to convince people that it’s okay.”
Author: Radhika Viswanathan
Read More