Symptoms of the novel coronavirus can vary a lot, if an infected person experiences them at all.
What are the signs you have been infected with the Covid-19 coronavirus? That’s become a surprisingly tricky question to answer, and it’s hampering the fight against the disease.
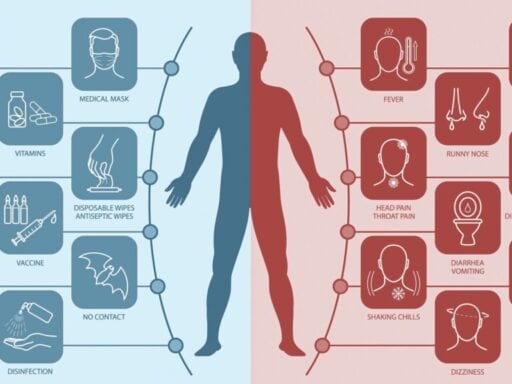
The Centers for Disease Control and Prevention (CDC) reports that the main symptoms of the illness are fever, coughing, and shortness of breath, appearing between two and 14 days after exposure.
However, some patients infected with SARS-CoV-2, the virus that causes Covid-19, have experienced completely different symptoms, like vomiting and loss of taste and smell. Some people’s Covid-19 symptoms overlap with those of other illnesses like influenza, making these infections hard to distinguish without testing. And some infected patients have reported no symptoms at all.
“As this pandemic unfolds, it’s becoming very clear that the symptoms of Covid vary quite a lot from person to person, and there are a lot of symptoms that we previously didn’t appreciate were related to Covid,” said Andrew Chan, a professor of immunology and infectious disease at the Harvard TH Chan School of Public Health. “As a result, it’s really put us behind in our ability to identify people with Covid infections, and probably resulted in a lot of people walking around with Covid and not knowing it.”
That has made responding to the crisis all the more frustrating and confusing for health officials, particularly in the United States, where tests for the virus remain scarce. Symptoms are an outward sign of the illness, and in a pinch can serve as a proxy for a test. Many hospitals are already telling patients with Covid-19 symptoms to presume they have the virus and to self-isolate, not even testing to confirm the presence of the virus.
A cluster of symptoms can highlight an emerging hotspot for the virus within a population. But without a clear picture of how Covid-19 manifests, it’s difficult to even approximate the true extent of the pandemic. And without a sense of what to look for, it’s hard for health workers to take proper precautions and offer the right treatments to their patients.
As a result, many communities have been forced to resort to blunt, blanket, and disruptive measures to contain the pandemic, like shelter-in-place orders. Relaxing these restrictions would require a major effort to test the public for the virus, trace movements, and build up health care capacity with beds, ventilators, masks, and workers. Yet there are parts of the US that have yet to impose even these crude measures to limit the spread of Covid-19.
Nonetheless, researchers are coming up with new ways to track the virus, going back to patient records to see what signs are associated with the illness. They’re also asking people to self-report their symptoms and tracking them with a mobile app. They’re finding that some mild, easily brushed-off symptoms could actually be a harbinger of the disease. This knowledge could help slow the pandemic and reveal new approaches to fighting the virus.
Some symptoms of the Covid-19 coronavirus are common, but milder signs are hard to track
Many of the guidelines for Covid-19 symptoms are based on what scientists have learned from past cases, particularly China, where the virus emerged and spread rapidly in January and February. The World Health Organization, for instance, looked at more than 55,000 confirmed Covid-19 cases in China. They found in February that the most common symptoms were fever (87.9 percent of confirmed cases) and dry cough (67.7 percent) — followed by fatigue (38.1 percent), sputum [phlegm] production (33.4 percent), shortness of breath (18.6 percent), sore throat (13.9 percent), and headache (13.6 percent).
But the patients they looked at weren’t necessarily representative of everybody who had the virus there — just the ones who received testing and treatment. In the study, about 80 percent of the patients had mild to moderate disease, 13.8 percent had severe disease, and 6.1 percent were in critical condition.
It’s likely that many infected patients with very minor or no symptoms were not captured by the study, which would mean their symptoms (or lack thereof) were underrepresented in those statistics.
Other studies have shown that symptoms such as gastrointestinal problems could herald the illness. A preliminary non-peer-reviewed study of 204 patients in China found that more than half of them experienced symptoms like diarrhea, vomiting, and abdominal pain.
Another preliminary study, this time from Germany, found that some Covid-19 patients had symptoms more like that of the common cold, like a runny nose. Researchers in Italy also reported that feelings of discomfort and malaise were associated with Covid-19. And doctors in the US have described neurological symptoms like confusion and seizures in some Covid-19 patients, particularly in the elderly.
These vague and sometimes contradictory symptoms may reflect how the virus interacts with underlying conditions in some patients, like diabetes and high blood pressure, or just differences in susceptibility. This kind of variation is a phenomenon physicians have already seen in other infections.
“For example, for influenza, most people will show up with fevers, body aches, and malaise. But a smaller subset of people will show up with diarrhea and vomiting,” said David Pride, associate director of microbiology at the University of California San Diego, in an email. “What we are experiencing with Covid-19 is probably just mirroring what we see in a number of other illnesses where it affects a subset of people in different ways.”
There’s also a huge range in how severe Covid-19 can be, even within certain subgroups. There are elderly patients who have shrugged off the virus. There are children that have died from it.
Many of these reports of less-common symptoms still need wider validation before they can be used as clinical guidelines. But they illustrate just how confusing it can be for patients and doctors to track Covid-19 without adequate testing.
A smartphone app has uncovered another likely symptom of Covid-19: A loss of taste and smell
In recent weeks, there have been murmurs that anosmia, a loss of the sense of smell, and ageusia, a loss of the sense of taste, could signal a Covid-19 infection. Utah Jazz player Rudy Gobert, who tested positive for the virus, said on Twitter that it was one of his most noticeable symptoms. The son of UK sports broadcaster Gary Lineker quaffed vinegar and lemon juice on Instagram to show off his loss of taste after getting Covid-19.
Doctors at the British Rhinological Society said in March they noticed “a rapidly growing number of reports of a significant increase in the number of patients presenting with anosmia in the absence of other symptoms.” Writing in the BMJ, researchers at Newcastle University said, “[T]here is now enough evidence to take this symptom much more seriously.”
Researchers in the United Kingdom recently bolstered that idea with data. Using a Covid symptom tracker app for smartphones launched on March 24, scientists pooled more than 1.5 million daily user reports of their symptoms or lack thereof. They found that a peculiar loss of taste or smell had strong links to testing positive for Covid-19.
“The strongest association between any of those symptoms and having a positive test was having a loss of smell or taste,” said Tim Spector, a professor of molecular epidemiology at King’s College London and lead researcher in the study.
In the study, 579 app users reported testing positive for Covid-19. And 59 percent of those said they lost their sense of smell or taste. That’s a higher rate than the Covid-19-positive app users reported for fever or any other symptoms.
The likely mechanism here has to do with how the SARS-CoV-2 virus works. Researchers in the US and UK reported in a preliminary study that the virus attacks cells associated with smell in nasal passages, in both mice and humans. That “could lead to anosmia or other forms of olfactory dysfunction,” the researchers wrote.
Spector cautioned that being unable to taste your coffee or smell wildflowers is not a definitive sign of Covid-19. A loss of taste and smell is associated with other upper respiratory tract infections as well as some allergies. In most cases, the loss of these senses isn’t permanent.
That’s why Spector’s team used their app data to build a model of what combination of symptoms was most closely associated with a positive virus test rather than examining any individual symptom.
Using the model, Spector and his team calculated that among the 400,000 app users who self-reported symptoms but did not get a Covid-19 test at all, about 50,000 of them were likely infected with the virus.
In places that lack adequate testing, Spector said this kind of symptom tracking could at some point serve as an early warning sign of a rising wave of Covid-19 — and allow potentially infected people to take precautions like self-isolation. And since they found that lost taste and smell can precede other symptoms by weeks, this could give health workers longer lead time to anticipate a spike in hospital visits. “We liken it to a radar,” Spector said.
The research is still in its early stages and may not be suited for making treatment decisions for individual people. But symptoms like anosmia could possibly be added to guidelines that determine who should be tested for Covid-19 or take precautions.
Spector also noted that the data from the app is skewed toward people who say they’re between 20 and 60 years old. Older people who may not typically use smartphones are underrepresented in his data. So are people in rural areas of the UK (the app just launched in the United States this week).
However, as more people sign up for the app, both those who are sick and those who are well, researchers can get a better picture of the pandemic and answer critical questions about the dangers of the virus, who is most at risk, and how best to limit its spread.
Spector is also collaborating with Harvard’s Chan and other researchers on the symptom-tracking app. Chan said that one of the key benefits of widespread symptom tracking is not necessarily finding the specific symptoms but being able to identify a sudden spike in symptoms, whatever they may be.
“If it’s just one person that feels this way, we don’t know what to make of that,” he said. “But if many people are feeling the same way with subtle symptoms then that is something that’s really worth sitting up and taking notice about.”
People transmitting Covid-19 before they have symptoms is a huge public health threat
Another complicating factor about Covid-19 is that people can spread the virus before they have symptoms, which can take up to two weeks to appear. And so people can transmit the disease to others unknowingly. Some virus spreaders may not ever feel sick throughout their entire infection.
According to the CDC’s Morbidity and Mortality Weekly Report from April 1, 2020, asymptomatic transmission “increases the challenges of COVID-19 containment measures.” Tactics like self-isolation or quarantines depend on early detection of potential infections, so without outward signs of illness, they become much less effective at slowing the disease.
It’s also still not clear just how many people are out there spreading the virus without noticeable symptoms. Chan said that it may be the case that many purported asymptomatic transmitters do actually have some symptoms but that they’re so mild that the infected don’t connect the dots between their experiences and Covid-19.
“There probably are some people who are truly asymptomatic, meaning they have the infection but feel perfectly well,” Chan said. “But there are probably people who have much more subtle symptoms or they may just assume that it’s related to something else.”
To find the people transmitting the virus without symptoms, researchers need widespread testing to confirm cases of Covid-19. Beyond the current genetic test that identifies active infections, scientists are also looking at serological testing, which can reveal who was previously infected with the virus (and may now have immunity to it). That information can help scientists see if patients overlooked any other potential signs of infection.
However, this would require public health officials to test more than the critically ill or health workers on the front lines; they will need far more widespread testing of the population at large to truly start to gain ground against the Covid-19 pandemic.
In addition to testing, safely lifting pandemic control measures like social distancing would require a massive coordinated effort to train health workers, to gather data, to trace contacts with the virus, and to manufacture all the equipment necessary. It would also require the public to remain vigilant about adhering to social distancing guidelines until then and to maintain good hygiene through tactics like proper handwashing.
But right now, the US is still struggling with widespread testing shortages. There are not enough testing kits to go around, as well as dwindling supplies of masks, gowns, and other personal protective equipment for workers collecting samples, as well as doctors and nurses.
That means health officials still have to make tough decisions about who to test, and they will likely remain in the dark about the true scope of the pandemic as cases and deaths continue to mount.
Author: Umair Irfan
Read More