Three systemic failures that explain the coronavirus’s terrible toll in US nursing homes.
The novel coronavirus has taken an unimaginable toll in America’s nursing homes and long-term care facilities. At least 25,000 residents and 400 staff members have died in the pandemic, according to new federal estimates.
To some degree, that toll simply reflects the sad realities of this crisis. Covid-19 is a disease that is particularly dangerous for the kinds of older and sicker people who live in nursing homes. About 80 percent of the deaths in the US — the latest count is more than 106,000, according to Johns Hopkins — have been people age 65 or older, per the CDC’s breakdowns. Preexisting conditions, particularly heart problems, also increase a person’s chances of developing a serious case or dying of the disease.
But the natural properties of the coronavirus alone are not enough to explain the losses in America’s long-term care settings, according to the experts I’ve spoken to. Also to blame are a series of policy failures — some predating the advent of the coronavirus pandemic, some of them made during the slipshod response to the outbreak.
“The huge number of nursing home Covid deaths is not simply a byproduct of a disease that spreads stealthily and disproportionately harms older adults,” David Grabowski, a Harvard Medical School professor who studies long-term care, told me. “Those factors have certainly contributed to outbreaks and deaths in nursing homes in the US and other countries, but it didn’t have to be this way.”
America has done a poor job funding and overseeing long-term care for decades, and there had not been adequate emergency planning for a crisis like the US is experiencing now with the coronavirus. And once the virus got here, the lack of a national strategy to ramp up Covid-19 testing in nursing homes and to provide protective equipment to staff made it easier for the virus to spread in these densely populated settings. Some state-level policy decisions, particularly to transfer recently recovered Covid-19 patients back into long-term care facilities, also exacerbated the risk to this population.
It all adds up to a devastating reckoning for a sector that is too often ignored in discussions about how to improve US health care. Here are three ways the coronavirus response went wrong in long-term care and what we might learn from it.
1) The US has not done a good job funding long-term care, exposing facilities to pandemics
Some of the structural problems that left nursing homes vulnerable can be traced back decades. The last significant reform to national long-term care policy was in 1987, according to Tricia Neuman, senior vice president at the Kaiser Family Foundation.
“One silver lining is maybe policymakers will focus on financing or quality protections moving forward, because they haven’t done it in quite a long time,” she said.
Nursing homes and other similar sites are reliant on Medicaid for most of their funding, and the state-federal program typically pays out at the lowest rates of any private or public health insurer. The US spends substantially less than most other rich nations, relatively speaking, on long-term care. Patients in the US also have a much lower share of long-term care costs covered by public programs.
“The lack of funding in nursing homes has really compromised the ability of nursing homes to implement strong staffing and infection control practices,” Grabowski says. “Medicaid is the dominant payer of nursing homes, and it has led to low payment rates for facilities which has translated to minimum wages for most direct caregivers.”
The long-term care industry itself lays much of the blame on these preexisting problems.
“The United States has under-invested in services for older adults for many years,” Katie Smith Sloan, president and CEO of LeadingAge, the association of nonprofit providers of aging services, told me in an email. “We lack a robust continuum of services that are adequately funded and that offer older adults supports to age well in all types of communities.”
And making matters worse, there had not been enough work done prior to the coronavirus to prepare nursing homes for the possibility of a pandemic.
“Each nursing home director has had to learn in almost an ad hoc way how best to manage this crisis,” Neuman said. “It’s not ideal to come up with best practices when you’re in the midst of a storm. Nursing homes were slammed with something they hadn’t anticipated.”
That structural failure is reflected in the fact that the quality of a nursing home, as measured by federal standards, hasn’t really seemed to matter in how it has been affected by Covid-19. The impact has largely been the byproduct of where the facility is located; high-quality and low-quality homes alike have been hit hard. Painfully few of them were adequately prepared.
And even as the threat of the coronavirus became clear, the federal government was slow to provide long-term care facilities with the resources and guidance they needed to fight it.
2) Nursing homes have lacked Covid-19 tests and protective gear
The experts and industry both said long-term care facilities have been hampered in their Covid-19 response by the difficulty in procuring tests and protective personal equipment, problems that have plagued the broader US response to the crisis as well.
“Long-term care providers are facing an unprecedented situation that has left them begging for testing, personal protective equipment and staffing resources,” the American Health Care Association/National Center for Assisted Living said in a statement. “Just like hospitals, we called for help. In our case, nobody listened for months, leaving a devastating consequence for our long term care providers. ”
The long-term care industry feels a palpable frustration that its call for a national testing and equipment strategy. From Sloan Smith of LeadingAge:
For the past two months, LeadingAge has called on Congress and policymakers to take a federal approach to prioritizing the distribution of PPE and of testing to protect older adults – a recognized at risk group – to no avail. The lack of comprehensive planning has meant that providers across the continuum have been forced to use precious staff time and resources scrounging for PPE for frontline workers and those they serve. The lack of comprehensive planning has resulted in a patchwork of approaches to testing and to resource distribution. We need staffing support during this time of incredible demands on front line workers and we need funding resources to bear the extraordinary burdens of this pandemic There is so much yet to do and LeadingAge continues to call on the federal government to provide leadership to protect older adults across a range of settings.
And the experts largely agree with them.
“The US has done the hard things such as locking down nursing homes to visitors and disallowing group activities and dining, but we have failed on more straightforward initiatives such as implementing surveillance testing and providing personal protective equipment,” Grabowski said. “We are not much further along today in these areas than we were in March.”
In mid-May, more than two months into the thick of the pandemic, the Trump administration said it wanted all nursing home residents and staff to be tested. But the US failed to meet the administration’s deadline for achieving that goal, and both the federal government and the states have still not given those facilities the money and the supplies necessary, based on my inquiries at the end of the month.
The collective bill for comprehensive testing is somewhere around $1 billion every week, according to Skilled Nursing News, and the plan to pay for it is a patchwork of Medicare covering patient costs and Medicaid covering staff testing. At the same time, some nursing homes are also starting to be hit with federal penalties for infection control failures.
“The administration has recommended that states and nursing homes implement testing and have adequate PPE but they have not put real dollars behind it,” Grabowski said. “A few states have made some headway in these areas, but most haven’t. Several states have also mandated testing and PPE but haven’t supported it with funding.”
3) States and nursing homes have made mistakes in handling Covid-19 patients
Nursing homes are not blameless, according to the experts I talked to. For example, in the early days of the pandemic, some facilities were reluctant to share information about their outbreaks in fear of being penalized by state or federal officials. A Maryland nursing home, with the most deaths in the state, did end up being fined for its failure to test residents, protect staff, or isolate people when they got sick.
That lack of information may have hampered the government’s ability to identify the scale of the problem in nursing homes and marshal resources to fight it — or it would have, if there had been a stronger national strategy to respond to the pandemic.
“It’s very hard to direct resources to facilities if you don’t know where they’re most needed,” Neuman told me. “Had there been a national strategy to distribute tests and PPE, which there wasn’t, that effort would have been greatly enhanced by basic data.”
Some early state policy decisions were also mistakes. The most obvious was New York’s decision to send recovering Covid-19 patients back to nursing homes. The Associated Press reported at least 4,500 patients were moved from hospitals to nursing homes from late March to early May.
While there was a rationale for that policy — to clear space in hospitals when officials were worrying about a spike in serious Covid-19 cases — it has become clear the real effect was to bring the virus into facilities where vulnerable people were living.
“New York’s mandate that nursing homes accept patients from the hospitals was a mistake. New York took a hospital capacity problem and made it a nursing home capability problem,” Grabowski said. “Ideally, New York would have invested in Covid-specialized nursing homes and units around the state. Obviously, New York did not feel like they could do this quickly enough, but this goes back to an overall lack of preparedness. New York made a huge investment in hospital capacity. Why not make a similar investment in post-acute capacity?”
But every policy strategy comes with trade-offs. To create Covid-specialized nursing homes, Massachusetts decided to move people out of their existing homes. But that plan was quickly abandoned.
“This was a failure on two levels,” Grabowski said. “First, it is really harmful to move older adults across facilities. Second, it was quickly determined that Covid was in most nursing homes in Massachusetts already and the state couldn’t find a Covid-free facility.”
We do have an idea now of what effective coronavirus response in US nursing homes should look like, according to the people I spoke to:
- Adequate testing
- Adequate staffing
- Adequate protective gear
- Separating Covid-19 patients and the staff who work with them from non-Covid patients and staff
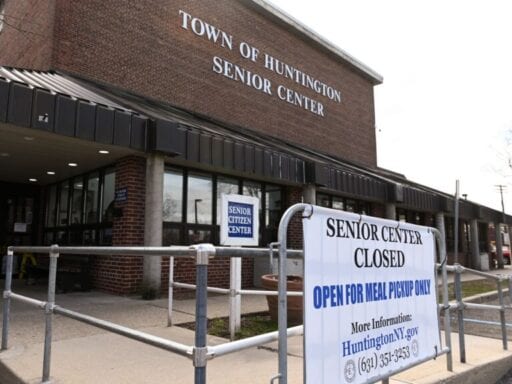
- Limiting outside access to the facility
Too many Americans have already paid the price for the country’s failure to create and follow that playbook. But, at that great cost, the best path forward has finally become clear.
This story appears in VoxCare, a newsletter from Vox on the latest twists and turns in America’s health care debate. Sign up to get VoxCare in your inbox along with more health care stats and news.
Support Vox’s explanatory journalism
Every day at Vox, we aim to answer your most important questions and provide you, and our audience around the world, with information that has the power to save lives. Our mission has never been more vital than it is in this moment: to empower you through understanding. Vox’s work is reaching more people than ever, but our distinctive brand of explanatory journalism takes resources — particularly during a pandemic and an economic downturn. Your financial contribution will not constitute a donation, but it will enable our staff to continue to offer free articles, videos, and podcasts at the quality and volume that this moment requires. Please consider making a contribution to Vox today.
Author: Dylan Scott
Read More