Not all experts are optimistic we’ll have a vaccine by the end of the year.
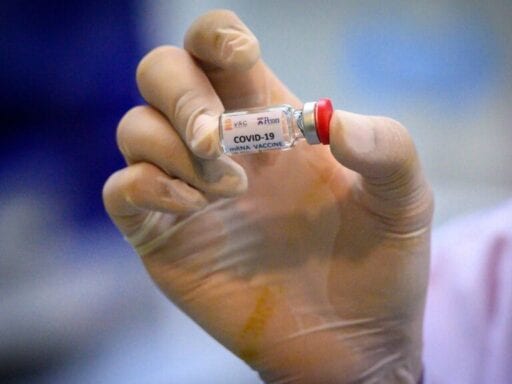
When will an effective Covid-19 coronavirus vaccine be ready for production for the general public?
Some top US health officials and researchers now expect one will be approved for use in less than a year. The specific estimates vary, but they say that the current push for a Covid-19 vaccine is unmatched in its scale and speed. With more than 140 vaccine candidates being studied, more than one is likely to pan out, they say.
“I am guardedly optimistic that by the end of 2020 we will have at least one vaccine that has been proven safe and effective in a large-scale trial,” Francis Collins, director of the National Institutes of Health, told New York magazine on July 1.
Similarly, Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases at NIH, said while there’s no guarantee that a vaccine will come to fruition, it is more likely than not.
He told a United Nations meeting July 8 that he has “cautious optimism that we will be successful at least in developing a vaccine with some degree of efficacy by the end of the year, the beginning of 2021.” It echoes similar comments he made to Congress in June.
There is also mounting political pressure for good news. As the United States has become the epicenter of the Covid-19 pandemic, leading the world in cases and deaths, the White House has been desperate for any beacon of hope in an election year marked by its disastrous pandemic response. On July 15, vaccine developer Moderna published some preliminary results in the New England Journal of Medicine showing that its vaccine candidate was able to generate antibodies to Covid-19 in test patients, a critical step toward demonstrating some immunity to the virus. President Trump hailed the announcement on Twitter:
Great News on Vaccines!
— Donald J. Trump (@realDonaldTrump) July 15, 2020
But does it make sense to bank on a vaccine by the end of the year?
After all, a vaccine developed in less than a year would break the record by a wide margin. The fastest vaccine ever developed was the mumps vaccine. It took four years, and the first iteration in 1948 only provided short-lived immunity. Many other vaccines have taken longer than a decade to come to fruition.
That’s why other officials have been hesitant to even suggest a timeline. “I can’t predict when a vaccine will be available,” Stephen Hahn, commissioner of the Food and Drug Administration told ABC’s This Week on July 5.
Rick Bright, the former head of the Biomedical Advanced Research and Development Authority, was also less sanguine. “A lot of optimism is swirling around a 12- to 18-month time frame, if everything goes perfectly,” he told lawmakers in May. “We’ve never seen everything go perfectly. I think it’s going to take longer than that.”
And Merck CEO Kenneth Frazier told Harvard Business School on July 13 that officials need to be more cautious about suggesting a timeline. “I think when people tell the public that there’s going to be a vaccine by the end of 2020, they do a grave disservice to the public,” he said.
All the while, there’s been a flurry of activity among vaccine developers, with new announcements of positive results seemingly every few days.
The emerging data certainly are encouraging and point toward the world developing a vaccine for Covid-19 in record time. But there is a much longer road ahead toward ending the pandemic, and there are many things that can still go wrong along the way.
Why some researchers think we’ll get a Covid-19 vaccine in record time
The urgency of a dangerous, fast-spreading virus has spurred an unprecedented amount of research. Scientists are pooling findings and resources from around the world on a scale never seen before. “There is a great deal of collaboration and coordination between the federal government, academic groups, and industry that we don’t typically see,” said Stephen Thomas, a vaccine researcher and head of the infectious disease division at SUNY Upstate Medical University.
There’s also a ton of money flowing into the endeavor. The United States launched Operation Warp Speed under the Department of Health and Human Services with almost $10 billion at its disposal. Its goal is to deliver 300 million doses of a Covid-19 vaccine by January 2021. The program is making investments not only in vaccine research, but in building factories and supply chains for multiple vaccines, with the expectation that not every vaccine effort will pan out.
The program recently awarded $1.6 billion to vaccine research firm Novavax. That’s in addition to funding Covid-19 vaccine development efforts at companies including Johnson & Johnson, Moderna, and AstraZeneca.
Companies and research groups in turn have been making progress. Pfizer and BioNTech announced earlier this month that early tests showed that their vaccine could generate an immune response. In addition to its recent promising preliminary data from phase 1 trials, Moderna also expects to begin its final phase of testing later this month. Meanwhile, researchers at the Jenner Institute at Oxford University said that they could have millions of doses of their vaccine candidate as soon as September under emergency approval.
Part of the optimism for getting a Covid-19 vaccine within months instead of years also stems from the virus itself. SARS-CoV-2, the virus behind Covid-19, comes from a family of coronaviruses like SARS and MERS that researchers have been studying for years. That’s given them a head start in examining the latest entrant.
And the fact that the vast majority of people infected with the virus recover on their own shows that most human immune systems are capable of fending off this disease. It stands to reason then that a vaccine could be designed to train immune systems to keep Covid-19 at bay. That’s in contrast to a virus like HIV, for which very few people have natural immunity or resistance, so scientists have yet to develop a vaccine for the virus despite decades of effort.
The technology behind vaccines has also improved in recent decades. In particular, Thomas highlighted the rise of platform-based systems for vaccines. Rather than engineering a vaccine from scratch for every new virus, scientists are developing vaccines with standard parts that have a few components that can be tweaked to make it work for a specific virus.
“I kind of look at it as the platform is the car and the specific disease that you’re looking at, those are the passengers,” Thomas said. “Because you know how the car is built and you’ve manufactured the car multiple times before, there’s a lot less work that has to go into a developing a new car every time.”
For instance, companies like CanSino Biologics and Johnson & Johnson are developing vaccines for Covid-19 that use a different virus, the adenovirus, as a vector to deliver genetic material coding for SARS-CoV-2 proteins that will trigger an immune response. Moderna, meanwhile, is developing an mRNA vaccine, an even newer platform that allowed the company to move with breathtaking speed.
“Moderna went 66 days from the time the sequence of Covid was published to their first injection of a patient,” said Drew Weissman, a professor of medicine at the University of Pennsylvania whose research was licensed by Moderna.
Some of these platforms, however, have never been approved for human use, which means they need extensive testing. To this end, clinical trials are also speeding up. Regulators have allowed vaccine developers to combine phases of clinical trials or run them concurrently.
Right now, the vaccines are still being tested. They have to meet a higher bar for safety than a treatment for Covid-19. Since vaccines have to be administered to vastly more people than a treatment, including the healthy, any risks are magnified. So while the development process has accelerated, researchers say that there can’t be any compromise on safety.
Even so, some vaccine developers have already posted some encouraging results. Some companies have shown their vaccine candidates have few safety problems and found evidence that they could lead to effective immunity.
“I think the optimism is warranted,” said Anna Durbin, a vaccine researcher and a professor of international health at the Johns Hopkins School of Public Health. “We should be able to see efficacy results from two or more of those trials by the end of [2020].”
In sum, the record pace of research, the extraordinary amount of resources devoted to the effort, promising new technologies, and early positive results are leading some scientists to believe the world will have a Covid-19 vaccine in record time.
“I think it is likely we will have one or more vaccines available to the public by the first quarter of next year,” said Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, in an email.
Thomas estimated that it would take a bit longer. “I would be very surprised if there was a vaccine available before the second quarter of calendar year 2021,” he said.
There’s a lot that can still derail a coronavirus vaccine
Throwing an enormous amount of money and labor at the challenge of developing a Covid-19 vaccine is still no guarantee that one will be ready in record time, if one is made at all.
While the early results from vaccine trials are pointing in the right direction, they still need far more validation before they’re cleared for widespread use. That requires testing tens of thousands of human subjects. Figuring out the efficacy of a vaccine is particularly time-consuming because researchers have to compare a test group to a control group and see how they respond to natural exposures to Covid-19 over time. How quickly that happens can change depending on how prevalent the virus is within a given population. It can take months.
Scientists also don’t know for certain whether the presence of antibodies to SARS-CoV-2 confers immunity and they don’t know how long that immunity would last. That’s another factor that can only be revealed by waiting and seeing.
Though companies have been making promising announcements in press releases and the occasional pre-peer review paper, some are still being cagey with their data. “There aren’t a lot of results that have been posted,” Durbin said.
However, even if a vaccine is proven to be safe and effective by the end of the year, it can’t end the pandemic without a coordinated vaccination effort. Enough people have to be vaccinated within a population to build up herd immunity, making it so the virus can’t easily spread and so that even the remaining unvaccinated people are protected. Building up that capability will take time and at the outset, governments will have to make some difficult decisions about who is going to be vaccinated first. “Without question, we are not going to have enough doses for every single person in the world,” Durbin said.
Getting enough vaccines to end the pandemic will therefore require a global supply chain, gargantuan manufacturing capabilities, and thousands of people trained to administer the vaccine.
That might be the biggest vulnerability for the United States. The country is still struggling to test enough people for Covid-19 and is still having problems getting adequate personal protective equipment to health workers months into the pandemic. Tests and PPE are far less complicated to manufacture than vaccines, so logistical challenges may end up as a major obstacle to a vaccination effort.
So while a Covid-19 vaccine could arrive at a record pace, actually getting it to enough people to end the crisis could be a much longer ordeal. The science is solvable, but building the political will to use it effectively remains a stubborn hurdle.
Support Vox’s explanatory journalism
Every day at Vox, we aim to answer your most important questions and provide you, and our audience around the world, with information that has the power to save lives. Our mission has never been more vital than it is in this moment: to empower you through understanding. Vox’s work is reaching more people than ever, but our distinctive brand of explanatory journalism takes resources — particularly during a pandemic and an economic downturn. Your financial contribution will not constitute a donation, but it will enable our staff to continue to offer free articles, videos, and podcasts at the quality and volume that this moment requires. Please consider making a contribution to Vox today.
Author: Umair Irfan
Read More