The story of Jahi McMath, a teenage girl who died this summer, shows how painful a lack of consensus can be for families.
What is death, really?
Turns out there’s no true consensus among doctors, bioethicists, and philosophers. The way death is determined can even change as you cross state lines.
Is it when our brains completely shut down? Is it when parts of our brains stop working? Is it when our hearts or lungs stop working? Is it when we lose the ability to think?
The line can be blurry, especially now that we have technology to keep organs functioning. Because of these artificial ways of sustaining life, differentiating death from life sometimes falls outside of the boundaries of science, according to Robert Veatch, professor emeritus of medical ethics at Georgetown University and the senior research scholar at the Kennedy Institute of Ethics. “It reflects the intersection of medical science and philosophy and religion,” he said.
He believes that the question of whether someone has died is really: “What is important about an individual that makes him one of us? … It’s only in one in 1,000 cases, maybe, that we’ve got some of the key indicators of life but not others, and then we have a fight.”
Most recently, there was the case of 17-year-old Jahi McMath, who was first pronounced dead five years ago after a tonsillectomy in 2013 went awry and left her brain-dead.
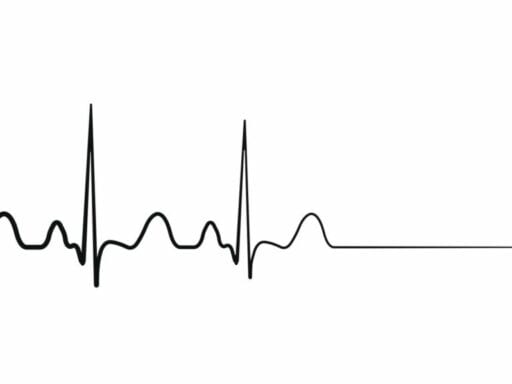
Brain death refers to the death of the brain stem: the part of the brain that controls basic body functions like breathing, heart rate, blood pressure, and consciousness.
But McMath was connected to a ventilator, and her heart continued to beat (the heart has an internal pacemaker, so it needs only regular oxygen to beat). Her mother, grandmother, and other family members believed that this meant she was still alive, and fought to keep her connected to a ventilator. The story became the subject of a lengthy New Yorker profile by Rachel Aviv.
/cdn.vox-cdn.com/uploads/chorus_asset/file/11920479/AP_18187743726813.jpg) Jeff Chiu/AP
Jeff Chiu/APAfter doctors in California declared her dead, McMath was transported to a hospital in New Jersey, which kept her on the life-sustaining treatment until she finally died of liver failure on June 22. But the battle is not over yet. According to the New Yorker, the family, who is African American, felt they were discriminated against (racism, no doubt, runs deep through the American medical system). McMath’s family is currently planning to file a wrongful-death suit against the hospital that declared her brain-dead, as well as a federal civil rights case.
Over the past few decades, other cases — like those of Terri Schiavo, Nancy Cruzan, Karen Ann Quinlan, and Marlise Muñoz — have sparked similar national debates about what rights an unresponsive person has, what rights their families have, and what a hospital’s responsibility is.
Typically, older people have advance directives or have otherwise made their end-of-life wishes known. So the ambiguous cases often involve young people whose parents disagree with doctors.
Most death determination is left to medical professionals, as it should be. But in these rare cases of uncertainty, when death actually has room for interpretation and the patient’s wishes are unclear, family members sometimes feel doctors don’t give their opinions enough respect.
Trying to understand what death means can help decide the best way to determine when someone has died. And beyond the medical ramifications, it turns out that untangling death actually tells us a lot about what it means to be alive.
The “official” way to determine death
The past century saw a burst in the development of medical technology that helps us sustain life. The “iron lung,” or precursor to the modern-day ventilator, was invented in 1928. The heart was first defibrillated — shocked back into its natural rhythm — in 1947, and we can now implant defibrillators right into the heart. Organ transplants also started in the mid-1900s.
Before all this technology, our organs and body parts were considered to be interdependent; when one part died, the whole body died. But these advancements changed the interdependent nature of our bodies; some parts could be artificially maintained even while other parts died. So the definition of death had to be clarified.
/cdn.vox-cdn.com/uploads/chorus_asset/file/11920301/shutterstock_692075692.jpg) Shutterstock
ShutterstockInitial drafts of a definition that incorporated brain death were criticized for sympathizing with the need for organ donors — a criticism that still exists for the current definition of brain death. After several iterations, the American Medical Association, the American Bar Association, and the President’s Commission on Medical Ethics finally developed the 1981 Uniform Determination of Death Act.
The Uniform Determination of Death is not a definition; it’s merely a guide that each state can adapt to determine how they legally decide whether someone has died. All 50 states have adopted it, with minor changes.
The act states: “An individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions, or (2) irreversible cessation of all functions of the entire brain, including the brain stem, is dead.”
In most cases, these criteria are easy to follow and don’t incite controversy.
The first category is usually pretty obvious; you can literally see a person’s heart or breathing stop. That’s how most people are declared deceased. But family members often find it hard to wrap their heads around what loss of brain function means.
“[Brain death] can be difficult for clinicians and families to understand. The patient looks the same immediately before and after the declaration of death by neurologic criteria, with the ventilator and whatever medications or interventions are sustaining cardiac function,” said Hannah Lipman, a physician and the director of bioethics at the Hackensack University Medical Center.
The criteria outlined by the Uniform Declaration of Death Act doesn’t cover some of the rarer cases, when people lose part or most of their brain function. For example, the act doesn’t say anything about people in persistent vegetative states (in which their brain stem still functions but they have no ability for higher-level thinking).
“It’s very confusing to people. Because on the one hand, personality is gone, the higher brain, the cerebrum,” said Steven Luper, a professor of philosophy at Trinity University who specializes in the philosophy of death. “But you could have a live brain stem. So they have a heartbeat, sometimes they can even breathe, they go through sleep-wake cycles, they can open their eyes.”
“So what we are in terms of having self-awareness, having mental ties to your various stages of life — that’s all gone,” he continued. “So you’ve got this clash of what appears to be a human animal — and death seems to be tied to that — and yet personality is removed.”
The problem with defining death
Even with the Uniform Determination of Death Act, the definition of death can be contentious for bioethicists.
“The best definition for death is a very trivial one: ceasing to alive,” Luper said. “And then, of course, that prompts us to try to be clearer on what it is to be alive.”
/cdn.vox-cdn.com/uploads/chorus_asset/file/11920265/shutterstock_615839501.jpg) Shutterstock
ShutterstockSo the definition of death really hinges on the question of what it means to be human. There are basically three schools of thought.
The first is that we are organisms, and that our existence is dependent on our organ systems functioning. “This group would say your brain could be completely gone, and gone for years, at least theoretically, and the individual could still be alive,” said Veatch.
This is considered a “circulatory-based” approach, according to Veatch. And a lot of religious people — including Jahi McMath’s family — follow these criteria.
So what would death look like for someone in this group?
“Death for an organism would be something roughly like its ceasing to engage in the various biological activities by which it develops and perpetuates itself, things like respiration and blood circulation,” said Luper.
This approach is essentially the first set of criteria outlined by the Uniform Declaration of Death Act.
The second method of defining who we are falls at the other end of the spectrum; it is the idea that a person is alive as long as any part of their brain is functioning. “That’s typically called the whole brain view now,” said Veatch. “And it’s the law almost everywhere in the world.”
This definition of being alive is why McMath was declared dead in California even though her heart was kept beating by a ventilator. But it is also why people in persistent vegetative states are not declared dead — they’re not brain-dead, but as far as we know, they also don’t have cognitive abilities. At the same time, people in persistent vegetative states have also recovered to either partial or full consciousness.
Imagine a person’s functioning and healthy brain is removed and placed into a new body, and their original body is destroyed. Is the person alive? If you agree with the first category of people, who think we are purely organisms, you would say not, since the original body doesn’t exist. If you fall in the second category and think our existence is dependent on our brains, you would say we are, since the brain has been transplanted. But neither answer seems quite right.
Enter the third view, which is more nuanced. This view says that certain parts of the brain are central to making us human, while other parts are not as important. For example, having higher brain functions such as personality and cognition, most of which are controlled by our frontal lobes, is more important than having a gag reflex or secreting hormones. But executing this practice is pretty complicated.
“If you think we’re self-aware beings, then, well, you’re gone as soon as parts of the brain permit self-awareness cease to exist, and then that’s all that’s relevant,” said Luper. “So they could easily say that death occurs, and yet the human animal is still there, alive.”
Within this third group still exists the question of what self-awareness means. Is it simply consciousness? Or something more than that? Would someone with severe dementia be considered self-aware?
Don’t worry, bioethicists and philosophers don’t really have an answer to all these questions either.
How leaving the decision up to families can help
All these debates are fascinating and important. But what’s the practical upshot? Most people who study death don’t think that we’re close to coming to a uniform consensus on what death really is.
This is a case where science does not have the answer. So why not leave it up to the patient’s loved ones? That is what Veatch believes.
“In my view, when we have those fights over what’s valuable about human life, there’s no way they’re going to be resolved,” he said. “So we might as well let [families] make their own value judgments based on their views of what’s important.”
Veatch argues that McMath’s mother’s beliefs should have been the final word: “For cases that are in the news today like Jahi McMath, as long as the mother was of the view that if she’s alive while she’s circulating blood, that’s good enough. She should have been classified as alive.”
And in the opposite scenario, if the family member of someone in a persistent vegetative state believes they should be taken off artificial life support, that should be allowed as well.
Veatch, along with physician Lainie Ross, recently delved into this argument — that families should have a greater say when their loved ones are unresponsive — in their book Defining Death: The Case for Choice.
McMath’s family transferred her from California to New Jersey, one of two states (the other being New York) where families are allowed to bypass the brain death criteria if it does not align with personal or religious beliefs. Instead, they can ask to use only the cardiopulmonary criteria: the rule that death comes with the irreversible stop of breathing and heartbeat.
Lipman works at the Hackensack University Medical Center in New Jersey. As a bioethicist, she is called to navigate these questions and typically sees between one and three families a year with religious objections to the brain death criteria. And if we’re looking for some uniformity in what all humans want, she’s found an answer: We want to be heard.
“When the Bioethics Consultation Service is asked to help address an ethics question, I go and do a lot of listening to the people involved. I’ll hear from the family to understand their experience, their belief system, and their understanding of the medical situation,” said Lipman. “I listen to the clinical team to understand what their perspective is. There’s no substitute for the magic that can happen when people listen to each other and understand each other’s experience.”
Yes, there are some challenges with having families decide whether they believe brain death should equate to death. It’s not clear if Medicaid should fund hospital stays after a person is declared brain-dead. (McMath’s mother funded her transfer to New Jersey via GoFundMe.) How long should a body be kept alive with machines? What if different family members have opposing views? What if the dying person is a registered organ donor?
More importantly, these complications around determining death usually happen when a person’s prognosis is dire. For loved ones, it’s not about a hope for a cure; rather, it’s about having the time to accept and grieve.
“I’ve worked with families whose religious beliefs do not allow for death to be declared by neurologic criteria,” said Lipman. “Who still understand that their loved one is very sick, dying, and not going to recover. They may ask that the ventilator be continued until cessation of cardiac function.”
Sometimes, giving the family the reins is about respect. The McMath family’s biggest complaint is that they did not feel their opinion was acknowledged. As Jahi’s mother told the New Yorker, “No one was listening to us, and I can’t prove it, but I really feel in my heart: if Jahi was a little white girl, I feel we would have gotten a little more help and attention.”
Perhaps the years-long emotional and legal battle could have been avoided had the family been allowed to come to terms with McMath’s death on their own accord.
“Explaining that process [of dying] to families, it really requires a lot of love, support, relationship-building, and trust, and understanding of values,” said Lipman.
Author: Radhika Viswanathan