The CDC found spikes in cases of syphilis, gonorrhea, and chlamydia — again.
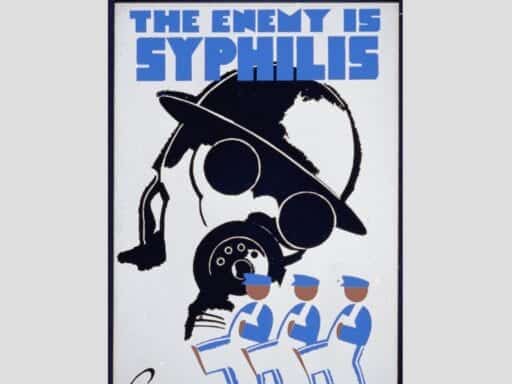
We don’t talk much about chlamydia, gonorrhea, or syphilis, in part because it can seem like they’re not big health issues anymore. But it turns out more and more Americans may be quietly suffering from these once nearly eliminated STDs.
According to a new report from the Centers for Disease Control and Prevention, there were nearly 2.4 million cases of chlamydia, gonorrhea, and syphilis reported in the United States in 2018 — the highest cumulative number ever recorded.
The leap in cases over the last few years is truly eye-popping. Between 2017 and 2018, the rate of:
- Gonorrhea cases increased by 5 percent, to 580,000 cases in 2018 — the highest number since 1991.
- Primary and secondary syphilis cases (the most infectious stages of the disease) increased by 14 percent to 35,000 cases — also the highest number since 1991. The total number of syphilis cases was 115,000.
- Chlamydia cases grew by 3 percent to 1.7 million cases — the most the CDC has ever reported.
To appreciate just how astonishing the trends are, consider that as recently as a decade ago, these STDs were at historic lows or nearly eliminated. Better screening and diagnostics helped identify cases and get people into treatment. Now, those efforts have been undermined by a lack of funding for STD prevention as well as peoples’ behaviors, which public health officials are scrambling to keep on top of.
Syphilis can show up on the body in sores and rashes. Gonorrhea and chlamydia can lurk with no symptoms. They’re all generally easy to cure with a prompt antibiotics prescription. But when left untreated, they can lead to infertility or life-threatening health complications, particularly in fetuses and infants. That’s what makes screening and access to health care so important.
“STDs can come at a high cost for babies and other vulnerable populations,” said Jonathan Mermin, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. “Curbing STDs will improve the overall health of the nation and prevent infertility, HIV, and infant deaths.”
African Americans and men who have sex with men have traditionally been the populations most plagued by gonorrhea and syphilis (and they’re still disproportionately affected). But other groups are now catching up too, especially women and babies in contracting syphilis.
What’s driving surging rates of STDs?
So what’s behind the spread of these diseases here? There’s no single explanation. Like most health trends, it’s complicated. But here are a few ideas, according to experts:
1) There’s been a rise in condomless sex among men who have sex with men.
Gay, bisexual, and other men who have sex with men are generally more at risk for STDs than women and men who have sex with women only. (The majority of new syphilis and gonorrhea cases occurred among men, and in particular, men who have sex with men.) And there’s been some concern about a shift toward riskier sexual behaviors in this group — like not wearing condoms — that may be contributing to the rise in STDs.
The reason for this shift has been explained by everything from the success in treating HIV (and therefore making unprotected sex less scary) to the advent of PrEP (pills that can prevent HIV). A systematic review published in the journal Clinical Infectious Diseases found that some PrEP users are having more risky sex — and are being diagnosed with more sexually transmitted infections.
HIV and syphilis are also interlinked: Some half of men diagnosed with a new syphilis infection also have HIV. And as these diseases spread in particular populations, like men who have sex with men, there’s a greater risk of them moving even further.
“The fear, which I share, is that we won’t contain syphilis among men who have sex with men,” Matthew Golden, director of the Public Health for the Seattle and King County HIV/STD control program, told Vox. And if the epidemic in men who have sex with men keeps growing, and spreads to women as well, “it won’t be possible to contain.”
2) STDs are spreading more broadly and into populations that weren’t traditionally affected — like babies.
The latest CDC numbers show a 40 percent increase in congenital syphilis cases from 2017 to 2018. So more and more women in America are getting syphilis these days, and they’re passing it to their babies. When an expectant mother is infected with the disease and goes undiagnosed and untreated, the bacteria can get into her bloodstream and move through her placenta to her baby. Congenital syphilis is associated with serious health consequences, like stillbirths and neonatal deaths. And newborn deaths linked to congenital syphilis — surged by 22 percent (from 77 to 94 deaths).
The large increase is being driven by only a handful of states. “Although most states reported at least one case of congenital syphilis, five states – Texas, California, Florida, Arizona, and Louisiana – accounted for 70 percent of cases in the US,” the CDC found.
Early STD detection and treatment can improve mom’s and baby’s outcomes. “There are tools available to prevent every case of congenital syphilis,” said Gail Bolan, director of CDC’s Division of STD Prevention, in a news release. “Testing is simple and can help women to protect their babies from syphilis — a preventable disease that can have irreversible consequences.”
But right now, not enough women in these syphilis hotspots are accessing testing and treatment.
3) With the rise of dating apps, sex is more readily available and more anonymous — and that makes it harder for health investigators to track outbreaks.
Health experts increasingly view apps and sites such as Tinder, Grindr, and OkCupid as enablers of high-risk sex, helping people meet and hook up more efficiently than ever before. The impact of these sites is so profound they are also transforming the way health officials track and prevent outbreaks.
These places, after all, had become important meeting points for men who have sex with men — the group most affected by the HIV epidemic.
Today, the public health focus has shifted to what some have called “digital bathhouses.”
“We used to think about what we can do with bathhouses and sex clubs to make sure people’s risk was reduced,” Dan Wohlfeiler, who works at the STD Control Branch of California’s department of public health, told Vox previously. “Now that dating sites and apps have become so common, we know we need to work with them.”
There’s just one problem: Many of the major dating networks don’t want to be involved in STD prevention, nor have they acknowledged the impact they’re having on public health.
4) The numbers may be higher because we may be better at detecting cases in some groups.
The rise in chlamydia — which overwhelmingly causes no symptoms but can lead to infertility in women — may be an artifact of better detection and screening. The CDC keeps finding that rates of chlamydia are highest among young women, the group that’s been targeted for routine chlamydia screening. So an increase could just mean more testing.
5) Cuts to public health funding mean fewer STD clinics.
Public health in the US — which includes operating STD clinics where people can get tested and into treatment — is historically underfunded. (As of 2012, only 3 percent of the health budget went to public health measures; the rest went mostly to personal health care.) And since the global financial crisis, public health funding has really taken a battering. There are 50,000 fewer public health jobs since 2008, and many STD clinics have had to reduce their hours or shut down.
STD clinics were a traditional safety net for people with these diseases. If those clinics continue to be harder to reach or vanish, finding and treating STDs will become even more difficult — and the diseases will continue to spread.
So in some ways, the STD increases across the country may have less to do with a changing sexual landscape and more to do with more limited access to sexual health care. “Once again, STDs are at crisis levels in the United States, reaching all-time highs for the fifth year in a row,” the Partnership to End the HIV, STD, and Hepatitis Epidemics said in a statement. “We cannot end the HIV epidemic on the back of an exploding STD epidemic, nor can we accept the fact that more and more babies are dying in this country as a result of congenital syphilis, an easily treated and highly preventable condition.”
Author: Julia Belluz
Read More